13/05/2025 – Regulatory challenges and biocompatibility tests — auf Deutsch lesen
Medical textiles in the global market
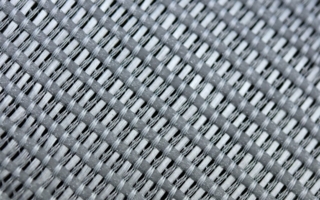
Technological advances and increasing demand for specialised textile applications are driving the growth of the medical textile industry and manufacturers must navigate the complex landscape of global regulations to ensure safety and efficacy.
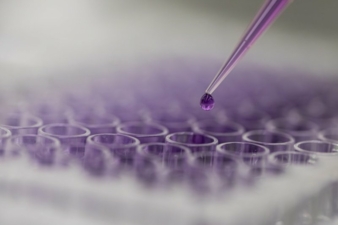
A proactive approach to biocompatibility and microbial testing can support product development and innovation and improve product safety and efficacy. © Hohenstein

Dr Timo Hammer is CEO of Hohenstein Laboratories, a testing and research service provider for softlines, hardlines and medical products. Headquartered in Bönnigheim, the family-owned company operates globally and employs around 1,200 people. Mr Hammer holds a doctorate from the University of Stuttgart-Hohenheim and is an expert in the development and testing of medical devices. © Hohenstein
Medical textiles can be divided into two categories: on the one hand, disposable items such as wound dressings or incontinence products. These items are used in patient care, where hygiene plays an important role and the material properties ensure optimum performance. The materials used for these textiles must fulfil strict legal requirements so that they are safe for direct contact with patients. Textiles also play an important role in filter systems, e.g. for respiratory and blood purification devices. In the other category, items such as surgical gowns and compression stockings are designed for repeated use and require durability and comfort as well as strict cleaning and sterilisation procedures. Surgical gowns, for example, are designed to be industrially laundered repeatedly while retaining their protective properties.
Legal framework in the EU
One of the biggest challenges is the different legal frameworks in the United States and the European Union. In the EU, medical devices are classified according to the Medical Device Regulation (MDR) 2017/745. This categorises products into four classes:
- Class I includes low-risk devices that are non-invasive and sterile or reusable, such as thermometers.
- Class IIa includes medium-risk devices such as catheters, surgical clamps and hearing aids.
- Class IIb devices represent medium to high risks, such as defibrillators and lasers.
- Class III devices such as heart valves and joint implants are considered high-risk devices and require a comprehensive assessment.
For Class I products, manufacturers can declare conformity themselves using the CE labelling procedure. The “Conformité Européenne” shows that a product fulfils the safety, health and environmental standards of the EU. For Class II and higher, verification by a notified body is required.
Classification in the USA
The U.S. Food and Drug Administration (FDA) uses a similar classification system for medical devices. For Class I devices, no independent testing is required prior to market release. For most devices, manufacturers must submit a 510(k) notification prior to market release. This demonstrates substantial equivalence to a legally marketed device by submitting clinical data and other relevant information. For critical medical devices (generally Class III) without comparator products, a more stringent authorisation process is required, which requires extensive clinical trial data to demonstrate safety and efficacy. These regulatory differences highlight the challenges and complexity manufacturers face in ensuring compliance and achieving market access for medical textiles in both regions.
Biocompatibility
Biocompatibility is an important aspect in the development and marketing of medical textiles. It determines how the materials interact with the human body. The tests usually include both in vitro studies (in a test tube or culture dish) and in vivo studies (on animals or humans). ISO standard 10993-1 outlines the required assessments. Chemical characterisation and three biological endpoints are standard for biocompatibility assessments for almost all medical devices:
- Cytotoxicity: evaluates the potential of a material to cause cell damage.
- Irritation: evaluates whether a material causes a localised inflammatory reaction.
- Sensitisation: determines whether exposure to a material can lead to allergic reactions.
In the USA, the FDA prescribes specific regulations and standards for biocompatibility tests that are based on the standard required by the EU. However, it does not fully recognise all standards. In general, a lack of detailed information on materials can make it difficult to assess compatibility. It is advisable to check this early on in the development process in order to find suitable materials before the product is finalised. Additional tests can be carried out to assess the finished textile product. Failure to adequately assess biocompatibility can lead to adverse patient outcomes and regulatory consequences.
Ensuring safety
The removal of production residues, germs and other impurities is crucial in order to prevent infections and other negative effects. Both the European Union and the United States therefore have regulations and guidelines on the cleanliness, cleaning and disinfection of medical devices. The Medical Device Regulation emphasises the importance of biocompatibility and microbial limits. The FDA regulates medical textiles within a similar framework, but the emphasis on cleanliness and disinfection is formulated through the Quality System Regulation (QSR) and specific guidance documents.
Customised collaboration with testing laboratory
Medical technology is bringing ever better and faster solutions to improve patient care. Manufacturers who want to succeed in global markets need to take a holistic view that includes compliance with multiple standards. A proactive approach to biocompatibility and microbial testing can support product development and innovation and improve product safety and efficacy. Many medical device manufacturers therefore work with a testing laboratory that is already familiar with the maze of global regulations and develop a plan tailored to their needs and budget. This not only ensures that medical textiles comply with legal requirements, but also guarantees the safety of people in a vulnerable environment.